Definition of Irritable Bowel Syndrome (IBS)
Irritable bowel syndrome or IBS is an umbrella term used to describe a collection of gut symptoms including abdominal pain which is related to altered bowel habits, for which we cannot find a structural or organic cause. 1 in 7 people worldwide are thought to have IBS.
This can be a frustrating diagnosis which has actually now been reclassified as a disorder of the gut-brain-interaction.
We have made some great progress in recent years in terms of understanding IBS and its complexity which can be affected significantly by diet, stress, an individual’s thought process, behavioural responses to symptoms and postinfectious changes.
IBS can be categorised into the following subgroups, based on your poop-ing patterns:
- IBS-C (constipation predominant)
- IBS-D (diarrhoea predominant)
- IBS-M (mixed bowel habits)
- IBS-U (unclassified)
Symptoms of Irritable Bowel Syndrome (IBS)
As well as altered stool habits, symptoms can include:
- abdominal pain / cramps / discomfort
- bloating (A whopping 80% of people diagnosed with IBS report this!)
- distension
- incomplete stool emptying
- urgent stools
- flatulence
- heartburn
- reflux
- anxiety
- fatigue
- back ache
- urinary symptoms
- headaches
As the symptoms of IBS are similar to so many other gut conditions, it’s really important we rule out other conditions as a cause, before making significant dietary changes.
Tests and diagnosis
Coeliac screen
This is one of the most important points from this blog post and a key take home! The one essential test you should complete before making dietary changes is a simple blood test for Coeliac disease. For this test to be accurate you should be including gluten in your diet, the equivalent of around 2-4 slices per day for 4-6 weeks before your test! There are two tests your GP needs to complete:
1. Tissue transglutaminase (TTG)
2. Total IgA.
It is the second test which is sometimes forgotten and essential to ensure the first test is accurate and not showing us a false negative (i.e. looks like a negative result but could actually be positive!)
Blood tests
Full blood count including C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) or plasma viscosity.
These are general inflammatory markers and if raised can provide an indication that further tests are needed before diagnosing IBS.
Stool tests
If you have diarrhoea and are under 45 years old, your GP should also complete a stool test for faecal calprotectin, which looks at inflammation which is more specific to the gut and again could indicate further tests are needed as there could be another underlying condition.
Recommendations are slightly different if you are over 45 years old as there are many other factors which can affect this stool test.
We know that in IBS there is no damage to the tissue, but in other gut conditions there can be. Therefore, diagnosis is key to ensure that any tissue damage is being treated.
What causes Irritable Bowel Syndrome (IBS)?
The causes of Irritable Bowel Syndrome are different for every person. For some, symptoms appear all of a sudden and for others, there may be a slow increase or build up over time.
We know there are a number of mechanisms involved which can include:
- altered gut motility
- bacterial/microbiome changes
- infections
- increased gut sensitivity (visceral hypersensitivity)
- genetics
Irritable bowel syndrome treatments
IBS is considered a chronic (long-term) condition, symptoms can fluctuate over time. However, there are a number of dietary and lifestyle changes which have been shown to help improve symptoms.
The following “first line” dietary changes have been shown to be effective in around 50% of people with IBS. This means that for half of people with IBS they do NOT need to restrict their diet – it’s a common misconception that we put everyone on the low FODMAP diet! (More on that next week)
Changes should be applied consistently for 4 weeks to allow your gut to adapt and to monitor their effect.
- Caffeine: You don’t have to completely remove, try limiting to just 1 or 2 caffeinated drinks per day
- Sweeteners: avoid those ending in -ol (sorbitol, mannitol, xylitol …). Caution chewing gum, sugar free squash and low-calorie products!
- Water: Aim for 2L/day and sip slowly throughout the day if you can. This is especially important with constipation and drier stools.
- Fat: high fat foods such as pizza, burgers, cakes, crisps and pastries can increase symptoms in some people
- Fibre: spread your intake throughout the day. If you are struggling with constipation consider the slow addition of gentle fibres such as oats, flaxseeds/chia seeds or even a fibre supplement such as Psyllium husk or PHGG.
- Alcohol: keep to the guidelines of 14 units/week. This is the equivalent to 10 small glasses of wine/week or 6 pints of beer. Ensure you have at least 2 alcohol free days/week
- Fruit: a high concentration of fruit can be difficult for some people to tolerate. Stick to a max 3 fresh portions/day, splitting portions throughout the day
[elementor-template id=”3024″]
Dietary changes should always be looked at in combination with:
- activity levels
- sleep
- stress – this is a huge one, as the gut is connected to the brain via the gut:brain axis. We’ll look at this in more detail in another post. For now, remember that some deep, calming breaths each day before meals and before bed can be really helpful.
For some individuals, we do recommend additional treatment strategies. Those may include the low FODMAP diet (or a modified version of it), further investigation/tests, or even a referral to a gut-specialist psychologist where diet isn’t the main cause of symptoms. We have our very own psychologist starting at the clinic soon, so watch this space!
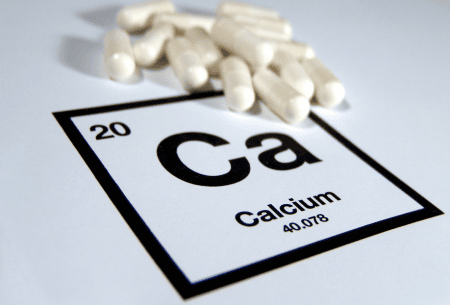
Over the next month, we’ll be covering the topics of the low FODMAP diet, the gut-brain axis, as well as key supplements that can be useful for managing symptoms. For more information on the programme of events for IBS awareness month take a look here.
This blog was authored by Lucy Kerrison, a gut specialist dietitian.