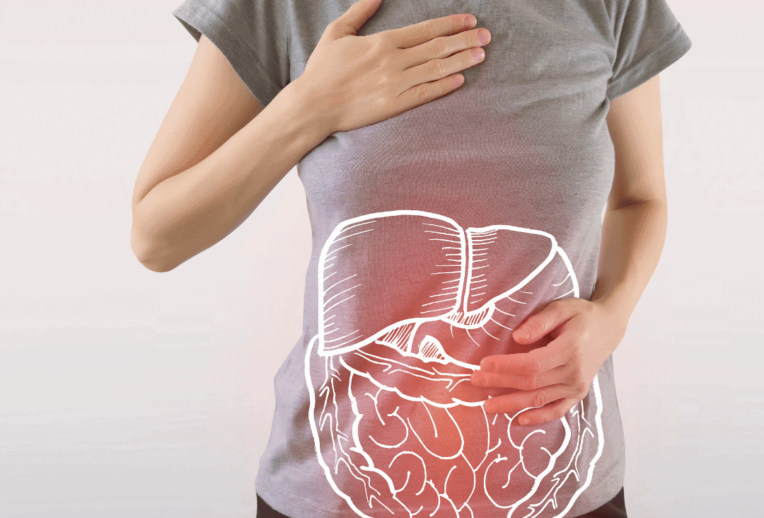
Ulcerative Colitis is an Inflammatory Bowel Disease (IBD) in which your immune system attacks the lining of your gut. This causes swelling and inflammation in your rectum and/ or colon (large bowel).
Why this happens is not clearly understood, but it is likely caused by a combination of factors such as genetics, gut microbiota, and environmental factors.
One of the most common questions I get asked in the clinic is ‘Was it something I ate that caused the onset of ulcerative colitis, or triggered a flare of symptoms? This is absolutely not the case!
Stages of Ulcerative Colitis
UC is a lifelong (chronic) condition, but everyone is affected by it quite differently. Most people go through periods of flare up, and remission:
Flare: A flare up is when your UC is in active inflammation. Symptoms can include diarrhoea, constipation, tiredness, tummy pains, and sometimes blood in your poo.
Remission: No active inflammation, symptoms are relatively well controlled.
Treatment
Treatment for Ulcerative Colitis may be with medicines, surgery, or a combination of both. This can vary depending on the site (where in your colon), and severity (how deep the ulceration, or how spread the inflammation might be). Your IBD and surgical team will help you to decide the type of treatments that best suit you.
Dietary advice
Due to inflammation, ulceration and above symptoms, UC can affect food choices, tolerance, and absorption of nutrients.
Below is some helpful advice to guide individuals through some nutritional considerations during a flare up period. Please bear in mind that this is general advice as every individual has different needs. This is why we would always encourage individuals to see a bowel specialist dietitian to ensure advice is tailored and provides an individual approach.
In remission:
When UC is well controlled and there is no active inflammation, you should aim to follow a healthy, balanced diet, rich in plant-based goodness and diversity.
Be sure to include the following food groups:
Starchy carbohydrates – wholegrain, wholemeal or seeded where possible – breads, pastas, cereals, grains, rice, potatoes, and pastas.
Lean protein – such as meat, chicken, fish, eggs, soya, tofu, tempeh etc.
Plant-based foods – try to include a diverse range of the six plant-based foods each day. This includes nuts, seeds, fruits, vegetables, wholegrains and legumes, as you can tolerate.
Vitamins and minerals:
Your body needs vitamins and minerals to work and stay healthy. Having flare ups and gut symptoms can change our tolerance (and sometimes absorption) to certain foods. People with UC should take care to ensure adequate intakes of the following:
Iron & Folate
Iron levels can become low due to reduced intake of iron containing foods, problems with absorbing iron, and blood loss in the stools. Try to include regular intakes of iron rich foods such as:
- Fortified breakfast cereals
- Green leafy vegetables
- Eggs
- Red meat
- Beans and pulses (if you can tolerate)
Consider having a piece of fruit containing vitamin C, or a glass of orange juice, with iron containing foods to help with absorption.
Vitamin B12
Vitamin B12 is found in foods such as:
- Meat
- Eggs
- Fortified cereals
- Cheese
- Fish
Mostly we get enough Vitamin B12 from our diets (though if you are following a vegan diet you may need to take a supplement).
Vitamin B12 is absorbed in a part of the gut called the ‘terminal ileum’. If you have inflammation in this part of your gut, or you have to have it removed, you may need to supplement with Vitamin B12.
Calcium
Calcium and Vitamin D play important roles in maintaining healthy bones.
Dairy foods such as milk, cheese and yoghurts contain excellent sources of calcium, as well as being a source of protein and other minerals. If you are following a plant-based diet, or limiting dairy due to symptoms, fortified alternatives such as soya, oat, rice and nut milks are a great source of calcium too.
Vitamin D
Vitamin D is found in foods such as oily fish, eggs, fortified cereals and fortified spreads.
Your IBD team will monitor your bloods and from time to time, you may need to take supplements to help correct any low levels.
In a flare up:
Though diet, or individual foods are never the cause of a flare, making changes to your diet can help ease symptoms. There is no specific diet to follow per se, as often the advice you are given will be based on your symptoms.
You may find it helpful to:
- Eat little and often, having nourishing meals and snacks regularly throughout the day
- Chew food well, taking time with meals and snacks
- Choosing high energy and high protein foods where you can
- Try to drink plenty of nourishing fluids
- Limit intake of spicy foods, caffeine, onions, garlic and alcohol
- Limit intake of fatty, greasy and heavy foods
- Reducing your intake of high fibre foods (such as wholegrain cereals, nuts, seeds, legumes and certain higher fibre fruits and vegetables) may help if you are struggling with loose stools
Surgery & Strictures
If you are having surgery, or you have strictures (narrowings) in your gut, you may be asked to change your diet. It is best to discuss with your Specialist Dietitian, as there really is no ‘one-size-fits all’ for this. In clinic, I like to work with clients and their IBD / Surgical teams, to ensure that they have a clear nutritional plan for before, during and after surgery. This may include focus on specific nutrients, use of supplements, liquid diets, or changes to fibre intake.
A final note
We know that receiving a diagnosis of UC can be particularly overwhelming and daunting to navigate the nutritional information available. Our Team of specialist dietitians at The Gut Health Clinic can support you each step of the way, so let us know if you want bespoke advice in clinic with one of our team or Book Here to arrange an appointment to speak with me.