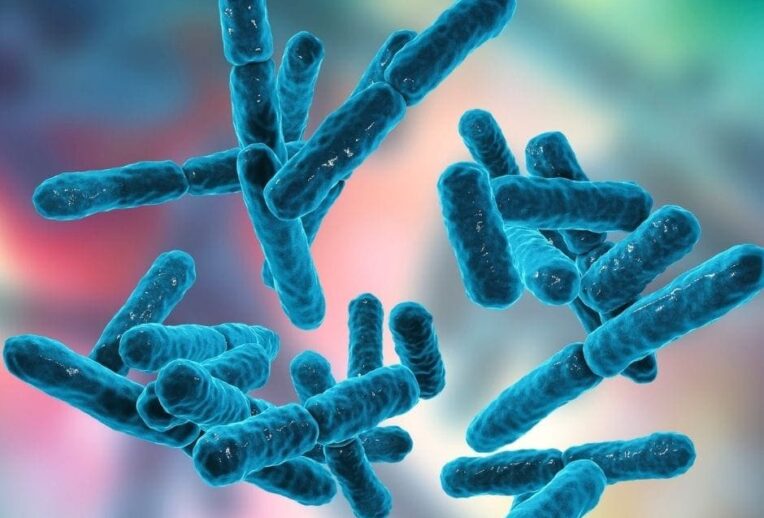
Probiotics has become a bit of a buzzword as of late – they’re advertised and sold everywhere with claims to improve various conditions or for general gut health. But what are they, and should you use them in IBS?
What are probiotics?
Probiotics are live microorganisms, which include bacteria and yeast. They have a positive effect within the large intestine to improve your health or reduce gut symptoms. This means that if you are adding them into your diet (through tablets, sachets or fermented foods), they must survive your entire gut: passing your acidic stomach and the length of your (incredibly long!) small intestine in order to reach your large intestine.
There are a number of enteric-coated tablets and sachets which we know can reach the large intestine, although some have far more evidence and research behind them than others. A quick google search will show you a dizzying array of combinations and formulas!
How do they work?
There are a number of mechanisms that occur, many of them poorly understood. What we do know is that probiotics can increase the production of short chain fatty acids (SCFA’s) which are the beneficial byproducts (also known as postbiotics!) which are responsible for the positive response within the gut. Note that postbiotic supplements have not been shown to be beneficial so save you money on these.
Probiotics can alter gut motility (hence helping with constipation or loose stools) and there is some really exciting research into psychobiotics, which have been shown to positively influence the gut:brain axis and mood (although not as a standalone treatment!)
Are probiotics helpful in IBS?
Whilst there are no official guidelines for recommending specific strains for IBS management, there is good evidence that probiotics can be beneficial for some people with IBS, and the British Society of Gastroenterology suggests they may be tried as first-line treatment (1).
HOWEVER it’s important to note that we all have very different guts and the probiotics which may benefit one person may not benefit another. In our clinic we can recommend probiotics based on your specific symptoms or IBS subtype, as well as considering your current diet and lifestyle.
If you’re keen to take a probiotic for your IBS you may benefit from choosing a multistrain brand which includes specific strains to suit your symptoms:
- Global IBS Symptoms
A recent study showed the strain Lactobacillus plantarum (Lp299v) to be effective overall in reducing global symptoms of IBS, however this does not mean it will work for all (2). There are many studies which suggest multistrain probiotics can be beneficial for global IBS symptoms. We can help guide you towards brands which are well researched and trusted.
- IBS-C (constipation predominant)
Strains which have been shown to benefit constipation (or IBS-C) include Lactobacillus rhamnosus GG (LGG), Bifidobacterium lactis BB-12, Bifidobacterium lactis HN019 (3).
- IBS-D (diarrhoea predominant)
Strains which have been shown to benefit loose stools include saccharomyces boulardii and bifidobacterium lactis HN019 (4) (5).
- Bloating
A recent review of chronic bloating showed that strains such as L.sporogens and bacillus coagulans can be effective to reduce bloating (6). Anecdotally, we can see improvements with a range of carefully selected multistrain probiotics.
[elementor-template id=”3024″]
Important considerations
Unfortunately, whilst there is evidence to support their use, that doesn’t mean it’s as simple as matching a probiotic to your symptoms for a quick fix. There are a number of people who will find probiotics do not improve their symptoms at all.
If you’re thinking about trying a probiotic then you need to ask yourself if you can afford it. It sounds obvious, but for some people the benefits of the probiotic cease when they stop taking it. Whilst we tend to recommend taking the probiotic daily for 4-12 weeks initially, it’s important to stop and evaluate its effect. Discontinue if it hasn’t helped you and consider an alternative strain, or something else to improve your symptoms, such as targeting the gut-brain connection.
Another point to think about is the route cause of your IBS. Theoretically, post-infectious IBS sufferers may be more likely to benefit from probiotics, than those who have not experienced a negative change in their gut bacteria (dysbiosis).
Probiotics can also be used to prevent the decrease in beneficial bacteria which occurs with the restriction phase of the low FODMAP diet, so your dietitian may recommend these for reasons other than symptom control (7).
Take home
Probiotics can be a helpful addition to some IBS sufferers, after taking into consideration current diet and lifestyle. Here at The Gut Health Clinic, we rarely recommend probiotics as a standalone treatment. If you do want to trial a probiotic for 4-12 weeks, be sure to choose one which is evidence based and specific to your symptoms!
This blog was authored by Lucy Kerrison, a gut specialist dietitian.