What is intestinal methanogenic overgrowth (IMO)?
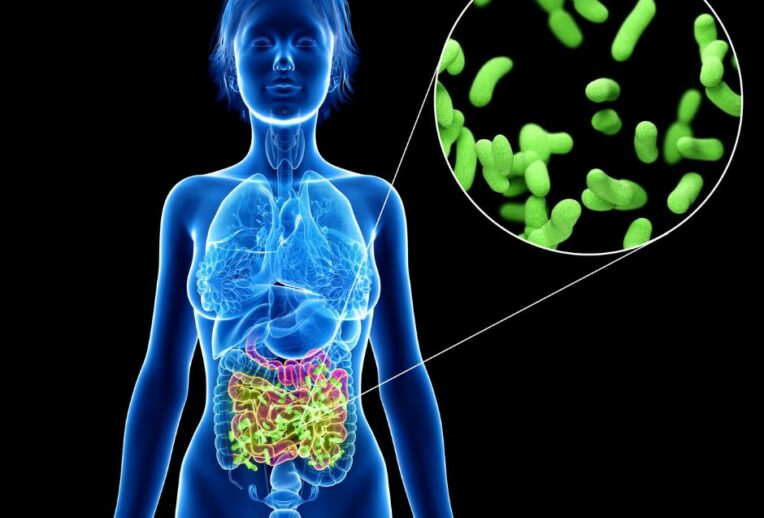
IMO is an overgrowth of microorganisms called the archaea throughout the gut. Archaea are a group of microorganisms that are similar to, but evolutionarily distinct from bacteria. This means that IMO is not the same as small intestinal bacterial overgrowth (SIBO), where the overgrowth is of bacteria, and which is limited to the small intestine.
The rise in breath testing and understanding of how the overgrowth of bacteria, fungi and archaea can impact the gut is pivotal in helping a cohort of people who experience gut symptoms such as changes in stools, bloating and abdominal discomfort.
High levels of bacteria in the small intestine, or methane within the small or large intestine, can increase gut symptoms in some people. We diagnose an overgrowth when we see a combination of symptoms, alongside a raised hydrogen (for SIBO) and methane (for IMO).
What are the symptoms of IMO?
There is some good evidence that raised methane levels are associated with an element of slow transit. The most common symptoms for IMO include bloating and constipation, but can also include other gut symptoms such as abdominal discomfort or even loose stools in some cases.
How is it diagnosed?
Breath tests are the most commonly used method for the diagnosis of SIBO or IMO. This is because they are less invasive and cheaper than other methods.
The process is outlined below:
- Referral should be from an experienced healthcare professional, this should not be a self-referral.
- For one or two days prior to the test you will follow a special diet which reduces all foods that can result in a rise in hydrogen levels within the body. Exercise and stress are also taken into consideration.
- The breath test should measure hydrogen, methane and carbon dioxide.
- You will be asked to breathe into a machine for around 20 seconds. This will be a baseline measure to ensure the diet has worked and if your initial hydrogen reading is not below 16, the results of the test should not be taken as accurate.
- After you have taken a baseline measure you will be given a solution (usually lactulose – a laxative, at a very small dose) which is fermented by bacteria and methanogens, resulting in a rise in hydrogen and/or methane gas. You will then continue to provide breath samples at intervals up to 90 or 120 minutes.
- SIBO is a slightly simpler diagnosis, as we can control hydrogen levels before the test and we can monitor at what time we see a rise in hydrogen levels. If we see a rise before 90 minutes, this is suggestive of bacteria in the small intestine (overgrowth), after 90 minutes, the bacteria is within the colon and not an issue.
- IMO is a more challenging diagnosis as our colonic levels fluctuate and we cannot control levels prior to the test. Methane levels above 10 during any part of a breath test are considered high. A diagnosis of IMO should be through an experienced professional as clinical judgement is heavily relied on.
So, what does a raised methane indicate?
There are multiple factors which affect your body’s methane levels and unlike hydrogen, they are not easily controlled. It is difficult to assess whether these methanogens are present in the large intestine or the small intestine. It is also difficult to control levels before a test and so the diagnosis of IMO can be challenging.
Your gastroenterologist may diagnose IMO, based on results and their clinical judgement.
What are the treatment methods for IMO?
Treatment can be through antibiotics, diet or a combination.
Antibiotics to treat IMO can be Rifaximin with Neomycin, or Metronidazole. Both Neomycin and metronidazole are systemic antibiotics, meaning they affect other areas of the body as well as just the gut, which could mean there is a higher level of side effects with these. There is no antibiotic treatment currently available for IMO which is not systemic as rifaximin alone has been shown to be ineffective in treating IMO.
In some instances a gastroenterologist will prescribe a motility drug such as prucalopride or linaclotide in order to get the gut moving again to prevent a recurrence. Laxatives may also be prescribed to target the constipation.
In terms of diet and lifestyle there are a number of factors to consider. One is your migrating motor complex (MMC). Your MMC is a digestive process which promotes the movement of food and waste products through your gut (including bacteria and archaea!) so they can either be absorbed and utilised or excreted as waste. It occurs predominantly in the stomach and small intestine during fasting and is interrupted during feeding. The third phase (of four) is the biggest sweeping movement and it occurs roughly every 90-120minutes in people. With this in mind, if you are someone who grazes throughout the day, you may not be giving your body many chances to reach that third stage of the MMC, which will help move bacteria and archaea out of the small intestine (e.g help to treat and prevent recurrence of SIBO and IMO).
As IMO is often associated with a slower transit and constipation, we also want to treat this constipation and prevent it reoccurring which can increase the risk of IMO returning.
Here are some tips for treating and preventing constipation:
- Ensure you are drinking enough fluid, this will help to soften the stool so it is easier to pass. Sip slowly and aim for 2-3L/day
- Slowly increase gentle and non-fermentable fibres in the diet. Fermentable fibres can exacerbate symptoms associated with IMO. You could try the addition of 2 x daily kiwi fruits, or a slow build up of chia/flaxseeds.
- Spread your fibre intake evenly throughout the day
- Get active – activity can help stimulate the bowel, treating and preventing constipation
See our previous post on constipation here which you may find useful.
Take home
The most common symptoms for IMO are bloating and constipation. However, the diagnosis remains difficult and controversial. If you are diagnosed with IMO, ensure this is from a trusted gastroenterologist and consider seeking dietetic support for symptoms, which are often linked with slow transit constipation.
This blog was authored by Lucy Kerrison, a gut specialist dietitian.